This article deals with the surgical options for presbyopia correction through the available methods for obtaining multifocality.
Versione in traduzione italiana
Introduction
Accommodation is the change in the dioptric power of the eye that allows us to focus from far to near(1). Presbyopia is the loss of accommodation, which begins early in life and becomes clinically manifest around age 40(1), enabling people to perform near vision activities without the use of glasses.
Presbyopia correction has been a challenge for refractive surgeons due to the fact that we have not achieved full restoration of accommodation and we have to rely in pseudo-accommodative procedures, which improve near vision by the induction of multifocality or increasing the depth of field(2).
It has been estimated that by 2020, 1.37 billion people will be affected by presbyopia(3), so, its correction is necessary as it decreases the quality of life(4) and represents an economic burden(5).
Presbyopia can be surgically corrected at the cornea with procedures like LASIK monovision, micro-monovision, presbyLASIK, Laser Blended Vision and corneal inlays; at the lens with multifocal or Extended Depth of Focus intraocular lenses ( EDOF IOLs), or with phakic multifocal IOLs. The selection of the procedure will depend on the patients’ age, expectations, daily activities and ocular comorbidities.
In this article we will discuss the surgical options for presbyopia correction.
Corneal procedures
The current corneal procedures for presbyopia correction are: LASIK monovision, micro-monovision, Laser Blended Vision, presbyLASIK and corneal inlays. The main advantages of these procedures are their reversibility, they are minimally invasive, and ideal for young presbyopes (<50 years). Ancillary tests like corneal topography and ultrasound pachymetry are necessary before surgery; patients with thin corneas or corneal ectasias are not good candidates for these procedures.
LASIK Monovision and micro-monovision
Monovision is an induced anisometropia in which the non-dominant eye is corrected for near vision and the dominant eye is corrected for distance vision. The degree of anisometropia increases depending on the patient’s age (-1.25 diopters (D) for a 40 year-old patient up to -2.50 D for a 65 year-old patient)(6). One of the main limitations of monovision is the loss of stereopsis, which is correlated with the degree of anisometropia.
In Micro-monovision the anisometropia induced in the nondominant eye is of -1.00 to -1.50 D and plano in the dominant eye irrespectively of the patients’ age(7). This degree of anisometropia allows the patient to retain a useful stereopsis(8).
Monovision is contraindicated in patients with strabismus, strong ocular dominance(9), truck or taxi drivers and airplane pilots(6).
Its simplicity, good clinical outcomes, and potential reversibility with a retouch using the excimer laser, makes monovision and micro-monovision highly efficient and frequently used by refractive surgeons.
PresbyLASIK
PresbyLASIK is an excimer laser procedure which creates a multifocal corneal surface(10), it has two main techniques: central and peripheral presbyLASIK. In peripheral presbyLASIK a central oblate zone is created for distance vision and a prolate peripheral for near vision(8). In central presbyLASIK a central hyper positive area is created for near vision and the periphery is for far vision(10) (Fig. 1).
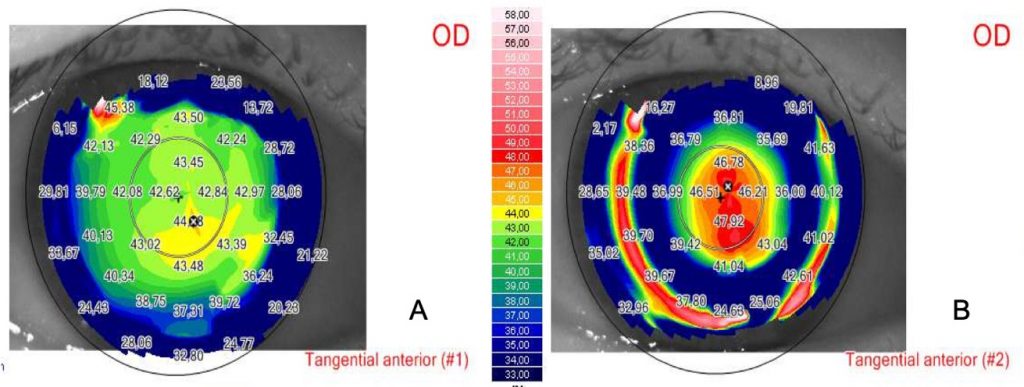
Due to the fact the peripheral presbyLASIK ablates a significant amount of corneal tissue in order to create a hyperprolate shape, central presbyLASIK is the most widely performed technique(11).
Some of the central presbyLASIK software available are: PresbyMAX (SCHWIND eye-tech-solutions GmbH, Kleinostheim, Germany), SUPRACOR (Technolas Perfect Vision GmbH, Munich, Germany), and AMO Visx hyperopia-presbyopia multifocal approach (AMO Development LLC, Milpitas, California).
The PresbyMAX software was developed by J. Alió and S. Arba; it can be used in emmetropic, myopic and hyperopic patients having good near and distance outcomes(12-16).
Although both techniques improve near vision, a loss of lines in distance vision has also been reported(17).
Laser Blended Vision
Laser Blended Vision combines a low degree of asphericity and micro-monovision in the near eye to achieve a good near and distance vision. This technique has good visual near and distance visual outcomes and can be performed in hyperopes, myopes and emmetropes(18-20).
We refer to the combination of monovision and corneal multifocality as “hybrid techniques”, LBV, Supracor and PresbyMAX software are within this group of hybrid techniques and they have improved the outcomes of corneal multifocality.(21)
Intracorneal Inlays
Intracorneal inlays have the advantage of being minimally invasive, reversible, and their implantation is easy, even though, its use has been questioned due to the decrease in contrast sensitivity, distance visual acuity and risk of corneal haze. All corneal inlays have to be centered on the first Purkinje reflex(22), and implanted under a stromal flap or within a stromal pocket made by the femtosecond laser(23) in the non-dominant eye(24) (Fig. 2).
Three different types of intracorneal inlays have been developed: corneal reshaping inlays, refractive inlays and small aperture inlays. We will discuss the latter because they are the most widely implanted inlays(22); corneal reshaping inlays (like the Raindrop, Revision Optics, Lake Forest, California, USA) have been phased out the marked due to an increased risk in corneal haze and loss of distance visual acuity, and refractive inlays (Flexivue (Presbia, Los Angeles, California, USA, Icolens, Neoptics AG, Hunenberg, Switzerland) have had contradictory results that have limited their clinical use.
Kamra
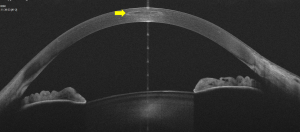
The Kamra inlay (Acufocus, Irvine, California, USA) improves near vision by increasing the depth of focus, it is an opaque inlay that has 3.8 mm diameter, a 1.6 mm central aperture and 8400 microperforations which allow an adequate nutritional flow through the cornea(25) (Fig. 3).
It can be implanted simultaneously with LASIK for myopes, hyperopes and emmetropes, with an improvement in near and intermediate visual acuity.(26,27) Some of the complications after the implantation of the Kamra inlay are: haze, photophobia, blurred vision, halos and refractive shifts(28-30); these complications have limited its use.
Multifocal and Extended Depth of Focus Intraocular Lenses
Replacing the crystalline lens by a premium IOL is the most definitive option for presbyopia correction as they correct distance, intermediate and near vision. They are the best option for hyperopes older than 50 years, and myopes older than 55 years.
Multifocal IOLs were introduced in the 1980s(31), and since then, their design has been improving in order to induce less photic phenomena while maintaining good visual acuities.
Considerations prior to Multifocal IOL implantation
A careful patient selection is mandatory in order to achieve good results.
Patients with type A personalities, as well as extremely demanding patients are not good candidates for a multifocal IOL. Patients with ophthalmologic conditions that decrease contrast sensitivity like advanced glaucoma or macular diseases are not good candidates for a multifocal IOL, as well as patients that lack the summation benefit of binocular multifocality (monofixators)(32), patients with irregular astigmatism, corneal and pupillary abnormalities(33). Astigmatism should always be corrected, so a topography is needed prior to surgery in order to choose a toric multifocal IOL.
Diffractive IOLs
Diffractive IOLs have rings on the surface which form a discontinued optical density(34). Apodized diffractive IOLs have a gradual decrease in diffractive step heights from the center to the periphery(33,34). Non-apodized IOLs have uniform step heights from the center to the periphery, such that light is equally distributed in both focal points independently of the pupil size(33,34). Some diffractive IOLs are: AT Lisa tri 389 MP (Carl Zeiss Meditec, Henningsdorf, Germany), FineVision (PhysIOL SA, Liège, Belgium), Acrysof IQ Pan 0ptix (Alcon Lab, Fort Worth, Texas, USA)
Refractive IOLs
Refractive IOLs have concentric zones of different dioptric power to achieve multifocality. Rotationally symmetric IOLs ( ReZoom, Abbot Medical Optics (AMO), Irvine, California, USA) achieve a good distance and intermediate vision, but a limited near vision. Other limitations include: pupil dependence, halos, glare and a high sensitivity of lens centration.(33)
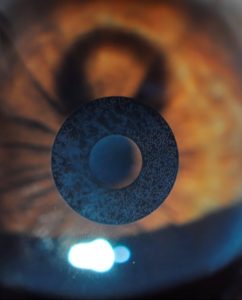
Rotationally asymmetric IOLs are the newer versions of refractive IOLs, they have an inferior segmental near addition and an aspheric distance-vision zone with a smooth transition between the two zones. They provide a good near, distance and intermediate vision with minimal photic phenomena due to the fact that light hitting the transition zone is reflected away from the optical axis preventing diffraction.(35) These IOLs include the Lentis Mplus (Oculentis GmbH, Berlin, Germany), and SBL-3 IOL (Lenstec. Inc., Christ Church, Barbados)
Extended Depth of focus (EDOF) IOLs
Extended depth of focus IOLs instead of creating several foci like multifocal IOLs, they create a single elongated focal point in order to enhance depth of focus; reducing photic phenomena.(36) Although intermediate vision is excellent with EDOF IOLs, near vision has a decreased quality(37,38) due to the induction of aberrations.(36) Pure EDOF IOLs are based on the pinhole effect like the IC-8 IOL (AcuFocus Inc, CA, USA), or on the spherical aberration like the Mini Well Ready IOL (SIFI, Catania, Italy).(36) Hybrid multifocal EDOF IOLs use chromatic aberration, a diffractive/refractive EDOF optic, or an additional power to increase the near vision.(36) The Tecnis Symfony ZXR00 (Johnson and Johnson Vision, Jacksonville, FL) and the At Lara 29 MP (Carl Zeiss Meditec, Jena, Germany) are an example of a diffractive/EDOF IOLs, the Lucidis (Swiss Advanced Vision, SAV-IOL SA, Neucha?tel, Switzerland) is a refractive/EDOF IOL, and the InFo – Instant Focus IOL (Swiss Advanced Vision, SAV-IOL SA, Neucha?tel, Switzerland) is a refractive-diffractive EDOF IOL.
Clinical and visual outcomes
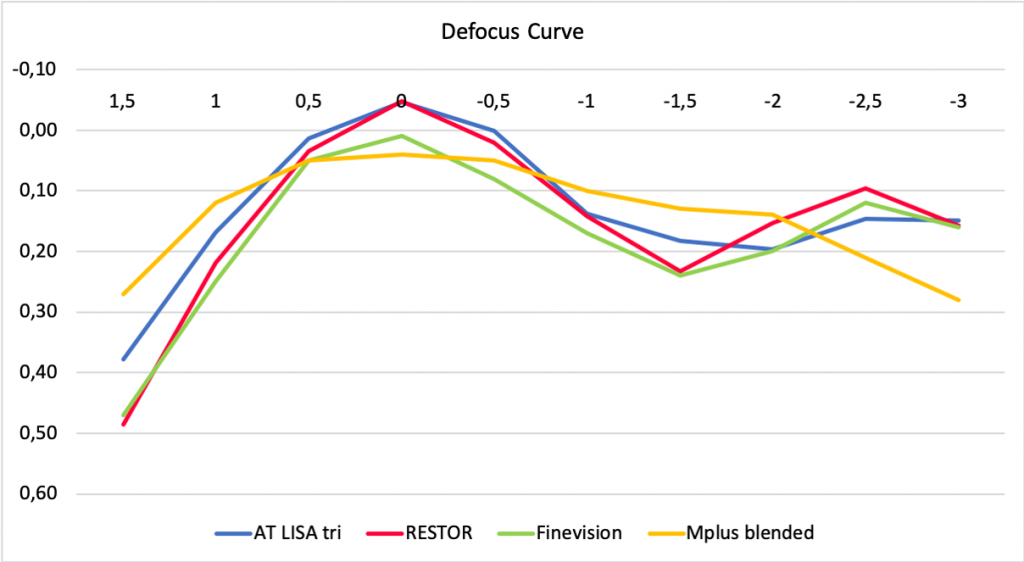
Patient satisfaction and visual function with multifocal IOLs are generally very good(39). Multifocal IOLs result in high levels of uncorrected distance and near visual acuity. Trifocal IOLs achieve better objective and subjective outcomes compared to bifocal IOLs(45). Distance and near visual acuity outcomes are generally better with diffractive multifocal IOLs compared to refractive multifocal IOLs(33).
One of effective way to compare premium IOLs is through the defocus curve, because we can compare the distance, intermediate and near vision achieved with each IOL. (Fig. 4).
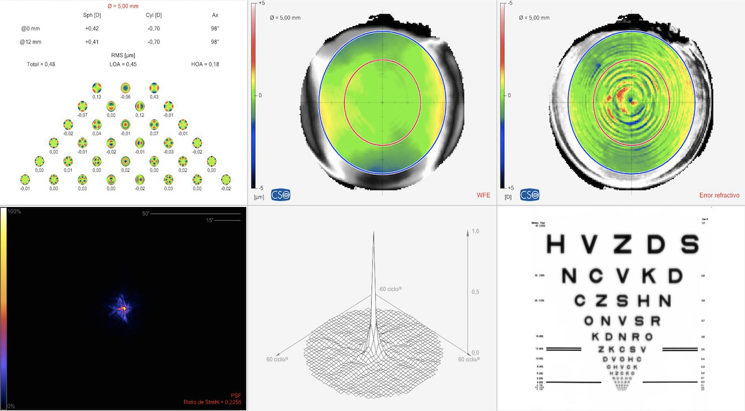
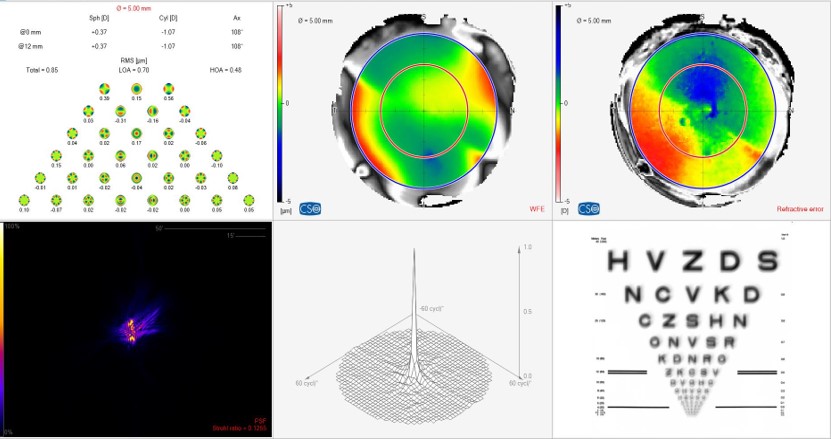
Higher order aberrations play an essential role in retinal image quality, and these can be induced by IOLs and affected by pupil size (Fig. 5 – 6). Compared to monofocal IOLs, multifocal IOLs typically result in more intraocular aberrations(46), although contrast sensitivity outcomes are comparable for monofocal and multifocal IOLs(47).
Reasons for patient’s dissatisfaction
Blurred vision is the leading cause of dissatisfaction which can be secondary to a large pupil, residual ametropia and astigmatism, posterior capsule opacification and dry eye(33). The second cause of dissatisfaction is the presence of photic phenomena like halos and glare, which appear more frequently after the implantation of a refractive IOL(33).
The most common reasons for multifocal IOL explantation and lens exchange are decreased contrast sensitivity, photic phenomena, neuroadaptation failure, incorrect IOL power, excessive preoperative expectations, IOL decentration and anisometropia(33).
Neuroadaptation
Neuroadaptation is a process in which the brain learns how to “correct” the image in order to use it properly so that the final perception is as real as possible. This process is easier in younger patients. It takes a minimum of three months for photic phenomena to lessen significantly, and it reaches its maximum point one year after surgery. Failure in neuroadaptation may cause distortion, confusion, a feeling of poor vision and the perception of glare(33). All patients implanted with a multifocal IOL go through a neuroadaptation process.
Our group has been a pioneer in treating neuroadaptation failure by changing the optic of the multifocal IOL, (for example, a refractive multifocal IOL for a diffractive multifocal IOL) having good results.
Future perspectives in rendering multifocality
The development of increasingly advanced technology for measuring and understanding aberrations, and its effect on visual quality have brought great advances in the development of intraocular lens implants. Hybrid multifocal EDOF IOLs are a promising technique that will promote the neuroadaptation process post-implantation. Focus now turns on allowing an individual to regain accommodation, whether by refilling the capsular bag with polymers that mimic the crystalline lens(48), and most especially to the creation of increasingly improving accommodative intraocular lens implants(49).
Conclusion
For now, most of the available methods for obtaining multifocality are adequate and effective. Treatment is individualized to meet the patient’s needs and maximize vision at all distances. Careful patient selection and screening, and thorough explantation of risks and benefits associated with each treatment option cannot be emphasized enough during the pre-operative planning period.
Authors: Veronica Vargas, MD1,2; Joan Balgos, MD1,2;Jorge Alió, MD, PhD, FEBO1,2,3
From:
1 Cornea, Cataract and Refractive Surgery Department, VISSUM Alicante, Spain.
2 Research & Development Department, VISSUM Alicante, Spain.
3 Universidad Miguel Hernández, School of Medicine, Alicante, Spain.
Financial support
This article has been supported in part by the Red Temática de Investigación Cooperativa en Salud (RETICS), reference number RD16/0008/0012, financed by the Instituto Carlos III – General Subdirection of Networks and Cooperative Investigation Centers (R&D&I National Plan 2008-2011) and the European Regional Development Fund (Fondo Europeo de Desarrollo Regional FEDER)
Corresponding Author:
Prof . Jorge L. Alió, MD PhD, FEBO
Calle Cabañal, 1 – Edificio Vissum. 03016, Alicante, Spain
E-mail: jlalio@vissum.com
Phone: 0034 672 398 765
REFERENCES:
1. Vargas V, Radner W, Allan B, Reinstein D, Burckhard D, Alió JL. Methods for the study of near, intermediate vision and accommodation: An overview of subjective and objective approaches. Survey of Ophthalmology (2018), doi: 10.1016/j.survophthal.2018.08.003.
2. Alió JL, Alió del Barrio JL, Vega-Estrada A. Accommodative intraocular lenses: where are we and where we are going. Eye and Vision 2017;4:16.
3. Holden, B.A., Fricke, T.R., Ho, S.M., Wong, R., Schlenther, G., Cronje, S., Burnett, A., Papas, E., Naidoo, K.S., Frick, K.D., 2008. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol 126, 1731-1739.
4. Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, Naduvilath T, Naidoo KS. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia. Systematic review, meta-analysis and modelling. Ophthalmology 2018, doi.org/10.1016/j.ophtha.2018.04.013
5. Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology 2015;122:1706-1710.
6. Goldberg DB. Laser in situ keratomileusis monovision. J Cataract Refract Surg. 2001;27:1449–55.
7. Reinstein DZ, Couch DG, Archer TJ. LASIK for hyperopic astigmatism and presbyopia using micro-monovision with the Carl Zeiss Meditec MEL80 Platform. J Refract Surg.2009;25:37-58.
8. Davidson RS, Dhaliwal D, Hamilton DR, Jackson M, Patterson L, Stonecipher K, et al. Surgical correction of presbyopia. J Cataract Refract Surg. 2016;42:920–30.
9. Ito M, Shimizu K, Iida Y, Amano R. Five-year clinical study of patients with pseudophakic monovision. J Cart Refract Surg [Internet]. 2012;38(8):1440–5.
10. Alió JL, Chaubard JJ, Caliz A, et al. Correction of presbyopia by technovision central multifocal LASIK (presbyLASIK). J Refract Surg 2006; 22: 453-460.
11. Wan Yin GH, McAlinden C, Pieri E et al. Surgical treatment of presbyopia with central presbyopic keratomileusis: One-year results. J Cataract Refract Surg. 2016;42:1415-1423.
12. Uthoff D, Pölzl M, Hepper D, Holland D. A new method of cornea modulation with excimer laser for simultaneous correction of presbyopia and ametropia. Graefe’s Arch Clin Exp Ophthalmol. 2012;250(11):1649–61.
13. Luger MH a., Ewering T, Arba-Mosquera S. One-Year Experience in Presbyopia Correction With Biaspheric Multifocal Central Presbyopia Laser In Situ Keratomileusis. Cornea. 2013;32(0):644–52.
14. Baudu P, Penin F, Mosquera SA. Uncorrected Binocular Performance After Biaspheric Ablation Profile for Presbyopic Corneal Treatment Using AMARIS with the PresbyMAX Module. Am J Ophthalmol. 2013;155:636–47.
15. Luger MHA, Mcalinden C, Buckhurst PJ, Wolffsohn JS, Verma S, Mosquera SA. Presbyopic LASIK Using Hybrid Bi-Aspheric Micro-Monovision Ablation Profile for Presbyopic Corneal Treatments. Am J Ophthalmol. 2015;160(3):493–505.
16. Chan T, Kwok P, Jhanji V, Woo V, Ng A. Presbyopic Correction Using Monocular Bi-aspheric Ablation Profile (PresbyMAX) in Hyperopic Eyes: 1-Year Outcomes. J Refract Surg. 2017;33(1):37–43.
17. Vargas V, Alió JL. Corneal compensation of presbyopia: PresbyLASIK, an updated review. Eye Vis 2017; 13:4-11.
18. Reinstein DZ, Carp GI, Archer TJ, Gobbe M. LASIK for presbyopia correction in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL 80 and VisuMax. J Refract Surg.2012;28(8):531-539.
19. Reinstein DZ, Archer TJ, Gobbe M. LASIK for Myopic Astigmatism and Presbyopia using Non-linear Aspheric Micro-monovision with the Carl Zeiss Meditec MEL 80 Platform. J Refract Surg. 2011;27 (1): 23-37.
20. Reinstein DZ, Couch DG, Archer TJ. LASIK for Hyperopic astigmatism and Presbyopia Using Micro-monovision with the Carl Zeiss Meditec MEL80 Platform. J Refract Surg.2009;25:37-58).
21 . Arba Mosquera S, Alió JL. Presbyopic correction on the cornea. Eye and Vision. 2014:1-10.
22. Konstantopoulos A, Metha J. Surgical compensation of presbyopia with corneal inlays. Expert Rev. Med. Devices 2015. 12(3), 341-352.
23. Garza EB, Gomez S, Chayet A, Dishler J. One-Year Safety and Efficacy Results of a Hydrogel Inlay to Improve Near Vision in Patients With Emmetropic Presbyopia. J Refract Surg. 2013;29(3):166–72
24. Whitman J, Dougherty PJ, Parkhurst GD, et al. Treatment of presbyopia in emmetropes using a shape-changing corneal inlay. One-year clinical outcomes. Ophthalmology 2016;123:466-475.
25. Lindstrom RL, Macrae SM, Pepose JS, Hoopes PC. Corneal inlays for presbyopia correction. Curr Opin Ophthalmol. 2013;24:281–7.
26. Tomita M, Kanamori T, Waring G, et al. Simultaneous corneal inlay implantation and laser in situ keratomileusis for presbyopia in patients with hyperopia , myopia , or emmetropia: six-month results. J Cataract Refract Surg. 2012;38:495–506.
27. Tomita M, Kanamori T, Waring G, Nakamura T, Yukawa S. Small- aperture corneal inlay implantation to treat presbyopia after laser in situ keratomileusis. J Cataract Refract Surg. 2013;39:898-905.
28. Alió JL, Abbouda A, Huseynli S, Knorz MC, Emilia M, Homs M, et al. Removability of a Small Aperture Intracorneal Inlay for Presbyopia Correction. J Refract Surg. 2013;29(8):550–6.
29. Shing Ong H, Chan AS, Yau CW, Mehta JS. Corneal inlays for Presbyopia explanted due to corneal haze. J Refract Surg.2018;34(5): 357-360.
30. Dexl AK, Seyeddain O, Riha W, et al. Reading performance and patient satisfaction after corneal inlay implantation for presbyopia correction: two-year follow-up. J Cataract Refract Surg. 2012;38:1808-1816.
31. Akella SS. Juthani VV. Extended depth of focus intraocular lenses for presbyopia. Curr Opin Ophthalmol 2018; 29:318-322.
32. Braga-Mele R, Chang D, Dewey S, et al. Multifocal intraocular lenses: Relative indications and contraindications for implantation.
33. Alió JL, Plaza-Puche AB, Fernandez-Buenaga R, Pikkel J, Maldonado M. Multifocal Intraocular Lenses: An Overview. Survey of Ophthalmology (2017), doi: 10.1016/ j.survophthal.2017.03.005.
34. Gooi P, Ahmed I. Review of Presbyopic IOLs : Multifocal and Accommodating IOLs. Int Ophthalmol Clin. 2012;52(2):41–50.
35. Moore JE, Mc Neely RN, Pazo EE et al. Rotationally asymmetric multifocal intraocular lenses: preoperative considerations and postoperative outcomes. Curr Opin Ophthalmol 2017, 28:9-15.
36. Kanclerz P, Toto F, Grzybowski A, Alió JL. Extended depth of field intraocular lenses: an update.
37. Alio JL. Presbyopic Lenses: Evidence, Masquerade News, and Fake News. Asia Pac J Ophthalmol (Phila). 2019;8(4):273-274.
38. Böhm M, Petermann K, Hemkeppler E, Kohnen T. Defocus curves of 4 presbyopia-correcting IOL designs: Diffractive panfocal, diffractive trifocal, segmental refractive, and extended-depth-of-focus. J Cataract Refract Surg. 2019;45(11):1625-1636.
39. Rosen E, Alió JL, Dick H, Dell S, Slade S. Efficacy and safety of multi- focal intraocular lenses following cataract and refractive lens ex- change : meta-analysis of peer-reviewed publications. J Cataract Refract Surg. 2016;42:310–28.
40. Alió JL, Pikkel J. Multifocal Intraocular Lenses. The Art and Practice. 2nd edition. Springer; 2019.378p.
41. Alió JL, Montalbán R, Peña-García P. Visual outcomes of a trifocal aspheric diffractive intraocular lens with microincision cataract surgery. J Refract Surg. 2013 Nov; 29(11):756-61
42. Venter JA, Pelouskova M, Collins BM, et al. Visual outcomes and patient satisfaction in 9366 eyes using a refractive segmented multifocal intraocular lens. J Cataract Refract Surg 2013; 39:1477–1484.
43. Savini G, Balducc N, Carbonara C, et al Functional assessment of a new extended depth of focus intraocular lens. Eye.2019 Mar;33(3): 404-410
44. Schallhorn SC, Teenan D, Venter JA, et al. Initial Clinical Outcomes of a New Extended depth of focus intraocular lens. J Refract Surg. 2019;35(7): 426-433.
45. Vargas V, Alió JL, Ferreira R, et al. Long-term objective and subjective outcomes following bilateral implantation of diffractive bifocal or trifocal intraocular lenses. Paper in peer review.
46. Ortiz D, Alió J, Bernabe?u G, Pongo V. Optical performance of monofocal and multifocal intraocular lenses in the human eye. J Cataract Refract Surg. 2008;34:755-762.
47. Cochener B, Lafuma A, Khoshnood B, Courouve L, Berdeaux G. Comparison of outcomes with multifocal intraocular lenses: a meta-analysis. Clin Ophthalmol. 2011;5:45-56.
48. Kook D, Kampik A, Dexl A, et al. Advances in lens implant technology. F1000 Med Rep. 2013;5(3). doi:10.3410/M5-3
49. Alió JL, Simonov A, Plaza-Puche A, et al. Visual outcomes and ac- commodative response of the Lumina accommodative intraocular lens. Am J Ophthalmol. 2016;164:37–48.
Dr. Carmelo Chines
Direttore responsabile
