Very myopic eyes are exposed to the risk of degenerative processes that can seriously impair vision.
Chorioretinosis and myopic macular degeneration are among the complications of progressive myopia that can seriously impair vision.
Myopia
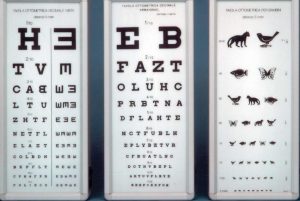
Myopia is a refractive defect whereby light rays are focused in front of the retina. Vision is therefore blurred at a distance and sharper up close.
'Myopia', in fact, comes from a Greek word meaning 'half-closed eye', as the myopic subject tends to squint in an attempt to focus images on the retina.
The causes
The causes are innumerable and include both environmental factors which factors hereditary e constitutional. In fact, this visual defect often occurs with similar characteristics among members of the same family.
In recent years, a link has been hypothesised between prolonged work at the video screen and increased myopia in adulthood.
Anatomically, the main causes of myopia can be:
1. an excessive length of the eyeball (axial myopia, the most common);
2. excessive curvature of the cornea or lens;
3. increased refractive power of the crystalline lens.
Types of myopia
Nearsightedness usually begins at school age and tends to increase during growth. It generally stabilises around the age of 25-30 years.
Depending on the number of diopters, myopia is considered:
- slight, up to 4 dioptres
- mediaup to 9 dioptres
- high, over 9 dioptres
In a fortunately limited percentage of cases, this visual defect presents itself in the form of degenerative myopiawhich begins at around 2-3 years of age and worsens with growth, following a process of retinal degeneration, which can lead to visual acuity values as low as -30 diopters.
Myopic macular degeneration
 Myopic macular degeneration or MMD (Myopic Macular Degeneration), is a frequent cause of low vision and visual loss in the adult population worldwide, particularly in East and South-East Asia.
Myopic macular degeneration or MMD (Myopic Macular Degeneration), is a frequent cause of low vision and visual loss in the adult population worldwide, particularly in East and South-East Asia.
According to a study, published in Investigative Ophthalmology & Vision Science, by the team of researchers led by Prof. Mukharram M. Bikbov, the prevalence of myopic macular degeneration at advanced stages (3 and 4) in the very elderly population increases 8.8-fold for every 1 millimetre increase in ocular axis length, with a prevalence of approximately 75% in individuals aged 85 years and over and a high risk of a marked deterioration of visual function.
Permanent degenerative changes
In general, eyes with high myopia are at risk of pathological myopia, a condition that leads to permanent degenerative changes, such as:
- Retinal atrophy: due to the abnormal elongation of the eyeball, which makes the retina thinner with the formation of atrophic areas associated with visual loss. The atrophy can affect any area of the retina, but when it occurs in the central part of the macula, it leads to a deterioration of central vision.
- Lacquer cracks: these are linear tears that occur in Bruch's membrane, between the retina and the choroid, and can also appear in the macula. They may also be associated with retinal haemorrhages, with or without choroidal neovascularisation (CNV).
- Choroidal neovascularisation (CNV): are blood neovases that can develop as a result of atrophy or lacker cracks and can involve the macula. Neovases are extremely fragile and have very permeable walls. Their presence can lead to the formation of scar areas and visual loss.
- Retinal detachment: the abnormal elongation of the eyeball and the consequent stretching of the retina increase the risk of retinal detachment from the ocular fundus, the most frequent symptom of which is the sudden onset of bright flashes and sparkles
In the aforementioned study of a sample of 1,526 individuals aged 85 years and over, 25.6% men, from the Russian republic of Bashkortostan, who were interviewed at home to collect biographical data and medical history, while they were summoned to the hospital for medical and ophthalmic examinations. Of those who performed all the protocol checks, individuals with stage 3 MMD (10 patients) and stage 4 MMD (11 patients) had significantly worse corrected visual acuity than participants without MMD. Among these patients, the prevalence of moderate to severe bilateral low vision was 40% (stage 3) and 64% (stage 4), respectively, while the prevalence of binocular blindness was 20% (stage 3) and 27% (stage 4). Among individuals with mild myopia, the prevalence of MDD was 0% for right eyes and 2% for left eyes. In the moderately myopic group, the prevalence of MMD increased to 8% (stage 3) and 11% (stage 4), while in the high myopes group it jumped to 78% (stage 3) and 75% (stage 4), respectively.
Myopic chorioretinosis
Myopic chorioretinosis is a degenerative ophthalmic disease that affects the eyes of patients with progressive myopia. This condition, characterised by the subtle thinning of the choroid, can lead to serious complications such as macular degeneration and retinal detachment.
Controlling the progression of myopia in children
 These results are fundamental to understanding the importance of controlling myopia in children to prevent the onset of retinal diseases in their adult life, also because most parents are not fully aware of the complications of high myopia.
These results are fundamental to understanding the importance of controlling myopia in children to prevent the onset of retinal diseases in their adult life, also because most parents are not fully aware of the complications of high myopia.
Each one diopter (1 D) increase in myopia over the course of a child's development increases the risk of myopic macular degeneration by 67% and the risk of retinal detachment by 30%, according to data published by Mark Bullimore and colleagues in Optometry & Vision Science. The same authors in a study published in Scientific ReportsThey predicted that by 2050 in the United States between 27% and 43% of uncorrectable low vision cases will be attributable to myopia.
In a 2019 study by Hansen and colleagues on a cohort of 1443 adolescents aged 16-17 years, the prevalence of myopia was 25%, with a doubled risk among those who spent a lot of time using digital devices rather than playing outdoors.
If we want to protect the health of our children's eyes, from an early age we should encourage them to go outdoors whenever possible: this will help them both to avoid the risks of sedentariness and overweight and to ward off dangers to their eyesight!
To answer many parents' questions about their children's eyesight, we point out:
- Children's eyes - Oculista Italiano
- Dysgraphia and visuo-postural defects - Oculist Italiano
- Myopia: a diagram to predict its development - Oculista Italiano
- Bikbov MM, Gilmanshin TR, Kazakbaeva GM, et al. Prevalence of Myopic Maculopathy Among the Very Old: The Ural Very Old Study. Invest Ophthalmol Vis Sci. 2024 Mar 5;65(3):29. doi: 10.1167/iovs.65.3.29. PMID: 38512243; PMCID: PMC10960226.
- Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci. 2019 Jun;96(6):463-465. doi: 10.1097/OPX.0000000000001367. PMID: 31116165.
- Bullimore, M.A., Brennan, N.A. The underestimated role of myopia in uncorrectable visual impairment in the United States. Sci Rep13, 15283 (2023). https://doi.org/10.1038/s41598-023-42108-y.
- Hansen MH, et al. Low physical activity and higher use of screen devices are associated with myopia at the age of 16-17 years in the CCC2000 Eye Study Acta Ophthalmol. 2019 10.1111/aos.14242.
