An undesirable outcome that risks compromising some of the visual benefits of the surgery.
Can cataract surgery induce severe forms of dry eye? If so, how often and under what conditions?
What is cataract
Cataracts consist of the partial or total loss of transparency (opacification) of the crystalline, the natural lens, located behind the iris, whose task is to converge light rays onto the retina.
The likelihood of developing cataracts increases with age, particularly after the age of 60, due to the physiological ageing of the crystalline lens. There are also congenital cataracts, i.e., present at birth, and cataracts of various origins such as those due to trauma, those from prolonged exposure to ionising radiation, and those induced by the intake of drugs used locally or generally (e.g., cortisone cataracts).
Risk factors for the development of cataracts include excessive and prolonged exposure to the sunlight. In addition, there are forms of cataract associated with other eye diseases, such as glaucoma and uveitis, or with systemic diseases, such as diabetes.
Cataracts are very often a bilateral disease, arising first in one eye and later developing in the other.
Symptoms
Cataracts sometimes take only a few months to develop, but most of the time the process takes years; sometimes it causes discomfort immediately, sometimes it does not cause discomfort for months.
The most common symptom is the progressive and gradual lowering of vision: the patient notices that his or her vision darkens and becomes blurred; he or she has difficulty reading, watching television, distinguishing objects at a small distance, driving especially at night.
The perception of split images and halos around light sources (headlights, lamps, etc.) is not uncommon.
Another symptom is the variation in visual capacity in relation to the intensity of ambient light.
Diagnosis
According to the 2014 SOI - AICCER guidelines for a correct diagnosis of cataract, the eye examination should include:
- general anamnesis, based on a medical history document drawn up by the general practitioner
- ophthalmic anamnesis, based on all clinical documentation relating to the patient's ophthalmic history.
- objective examination, noting the anatomical state of the visual apparatus with particular attention to all elements that may be relevant to surgery and in particular: presence of ocular pathologies associated with cataracts, dilatability of the pupil, explorability of structures posterior to the crystalline lens;
- functional examination: detection of distance and near vision with the best optical correction;
- biometrics;
- selection of the IOL according to the needs of the patient and the refractive status of the contralateral eye.
Treatment
Cataracts lead to visual problems that are reversible through surgical treatment by which the opacified lens is removed.
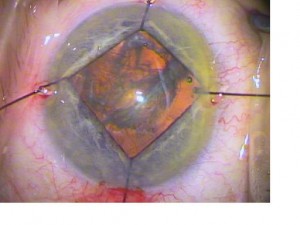
As a rule, the technique of phacoemulsification which involves the use of an ultrasound probe, which fragments and sucks out the opacified lens
Recently, cataracts have also been used in cataract surgery. femtosecond laser or femtolaser, which are able to ensure high standards of safety and surgical precision.
Once the cataract has been removed, an intraocular lens (IOL) or 'artificial lens' is implanted to restore satisfactory vision to the patient.
This lens, made of biocompatible materials, once positioned, remains fixed inside the eye and does not require cleaning or replacement. Modern IOLs can restore near-natural vision, provided that the other structures of the eye, in particular the retina, are healthy.
The most modern implantation techniques involve the use of lenses that can be inserted into the eye through very small incisions (mini- and micro-incisions), which do not require stitches.
Refractive cataract
The choice of the intraocular lens to be implanted is made taking into account the refractive defects from which the patient suffers (myopia, hypermetropia, presbyopia), so as to compensate for them in whole or in part and reduce or eliminate the need for glasses. This procedure is called refractive cataract.
Cataract surgery is preceded and followed by the administration of prophylactic pharmacological treatments, defined and approved by the guidelines of the major scientific societies, aimed at preventing and avoiding inflammatory and infectious complications, the most serious of which is postoperative endophthalmitis.
Prevalence
Cataract surgery is currently the most prevalent eye surgery procedure worldwide. On average, more than 26 million operations are performed each year worldwide, whereas in the year 2000 there were only 10 million, when according to the World Health Report 1998 it was estimated that there were already more than 19 million - 43% of the total number of blind people - who had been rendered blind in both eyes by age-related cataracts.
One of the causes is undoubtedly the extension of life expectancy, since cataracts are one of the most frequent diseases in the elderly over 65.
The 'dry eye' risk
Today, thanks to advances in surgical and diagnostic techniques and increasingly high-performance intraocular lenses (IOLs), cataract surgery has, in most patients, excellent refractive results. Some patients, however, develop major postoperative disorders, including dry eye syndrome or DED (Dry Eye Disease).
Symptoms
The most frequent symptoms, which tend to become chronic over time, are dry eye, foreign body sensation and visual fatigue. This symptomatic picture has a very negative impact on both quality of life and visual efficiency, with repercussions also on work productivity, making it necessary to identify strategies for the prevention and management of DED after cataract surgery.
In terms of pathogenesis, it is still not entirely clear what promotes the onset of DED after cataract surgery, with the consequence that no definite, evidence-based therapy has yet been identified. Furthermore, there is a lack of large, systematic studies on individuals who did not have DED prior to surgery and developed it after cataract removal.
Review and meta-analysis
On this sensitive topic, a 2022 review and meta-analysis attempted to shed light on prevalence, characteristics, risk factors and prevention measures.
Risk factors
The main risk factors have been identified in theadvanced age and in the sexas the women have a greater predisposition to postoperative DED. Specifically, Kohli et al. in a 2019 study showed that individuals over 60 years old, two weeks after cataract surgery, had worse results on OSDI, Schirmer, TFBUT, CFS (stereoscopic test), and TMH (tear meniscus height) tests. In addition, prolonged exposure to video terminalsespecially in more developed countries, may favour the occurrence of DED post cataract surgery, as illustrated by Villani et al. in a 2020 study.
Another important risk factor is the co-morbidityparticularly diabetes mellitus, autoimmune and neuropsychiatric diseases.
Favourable conditions for the onset of postoperative DED are also induced by certain drug therapiesin particular taking antihistamines, anti-reflux drugs, antidepressants, anxiolytics, sleeping pills, as well as hormone replacement therapy and thyroid hormone replacement therapy.
Prevalence and characteristics
According to data in the literature, the prevalence of post-cataract surgery DED in patients who had no dry eye symptoms prior to surgery ranges from 26.6% to 37.4%.
Regarding its course, some postoperative ocular surface changes generally tended to regress within the first month after surgery, however, most studies reported that DED parameters, including subjective symptoms, TFBUT, CFS, tear secretion volume, and Meibomian gland dysfunction (MGD) did not return to baseline throughout the duration of the study. Postoperative peaks in MGD severity were typically reported 1 week postoperatively, although they were also noted between 1 month and more than 1 year later.
Patients suffering from MGD prior to surgery were found to be more prone to the development of postoperative DED as MGD alters the stability of the tear film and the accelerated rate of tear evaporation and subsequent hydrolysis of tears inherent in this condition are highly likely to trigger the development of postoperative DED.
Prevention measures
The use of eye drops containing preservatives both pre- and postoperative, as they can cause ocular surface changes ranging from damage to apoptosis of epithelial cells, and reduced density of mucoid calycephalic cells.
A negative effect of prolonged use of the topical non-steroidal anti-inflammatory drugs (NSAIDs) in the postoperative period due to adverse effects on the density of conjunctival mucipolar calyciiform cells.
Appropriate preoperative management of MGD could help reduce the risks of DED after surgery.
On a general level, the use of filtered operating lights, a shorter duration of surgery, adequate intraoperative irrigation and very gentle handling of the ocular surface are conditions that can help minimise the risks of all postoperative complications and DED in particular.
See also our articles
Sodium hyaluronate and dry eye after cataract surgery - Oculista Italiano
Cataract surgery improves quality of life - Oculista Italiano
Cataract surgery: controlling ocular inflammation - Oculista Italiano
- Miura M, Inomata T, Nakamura M, Sung J, Nagino K, Midorikawa-Inomata A, Zhu J, Fujimoto K, Okumura Y, Fujio K, Hirosawa K, Akasaki Y, Kuwahara M, Eguchi A, Shokirova H, Murakami A. Prevalence and Characteristics of Dry Eye Disease After Cataract Surgery: A Systematic Review and Meta-Analysis. Ophthalmol Ther. 2022 Aug;11(4):1309-1332. doi: 10.1007/s40123-022-00513-y. Epub 2022 May 9. PMID: 35534685; PMCID: PMC9253209.
- Vision 2020: the cataract challenge. Community Eye Health. 2000;13(34):17-9. PMID: 17491949; PMCID: PMC1705965.
- Kohli P, Arya SK, Raj A, Handa U. Changes in ocular surface status after phacoemulsification in patients with senile cataract. Int Ophthalmol. 2019;39(6):1345-1353. doi: 10.1007/s10792-018-0953-8.
- Villani E, Marelli L, Bonsignore F, et al. The ocular surface frailty index as a predictor of ocular surface symptom onset after cataract surgery. 2020;127(7):866-873. doi: 10.1016/j.ophtha.2019.12.012.
