Antimicrobial resistance represents one of the most urgent and complex health challenges of our time, as it carries with it the threat of undermining the ability to treat even the most common eye infections, turning them into potentially devastating diseases.

The eyes, delicate and vulnerable by their very structure, are by their position frequently exposed to contact with bacteria and other microorganisms that can cause infections and, in the most unfortunate cases, infections resistant to traditional treatments.
With the abuse and misuse of antibiotics, the risk of eye infections becoming more difficult to manage is growing, endangering the sight and quality of life of millions of people.
This article aims to explore the causes of antimicrobial resistance, its effects on the eyes and effective strategies to protect visual health from emerging threats.
Understanding Antimicrobial Resistance
Antimicrobial resistance is a growing problem that affects global public health. It is, therefore, crucial to understand the mechanisms by which bacteria become resistant and the impact of this phenomenon on eye health and the health of the whole organism.
The problem of antimicrobial resistance, growing steadily on a planetary scale, arises when microorganisms become resistant to drugs, which used to be effective tools to eradicate them.
This phenomenon poses a serious threat to global public health, as the World Health Organisation (WHO) has repeatedly pointed out, as it can make common infections difficult to treat, increase the risk of spreading contagious diseases, and make some of them effectively impossible to treat.
The impact of antibiotic resistance extends far beyond the ocular field and in fact involves all clinical areas and, above all, has major repercussions on healthcare and economic systems.
Resistance leads to longer hospital stays, more expensive treatments and increased mortality. Moreover, resistant infections can easily spread among populations, further exacerbating the problem.
To effectively address this challenge, it is crucial to promote responsible antibiotic use on a global scale and to stimulate research into new treatments.
Only through global collaboration will it be possible to mitigate the impact of antimicrobial resistance.
How it Develops in Bacteria
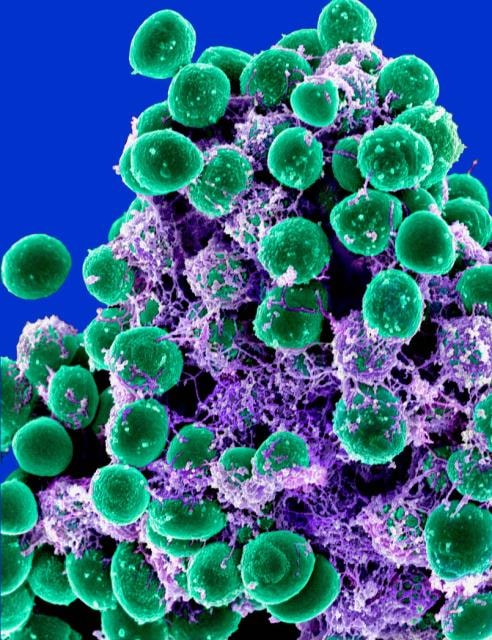
Bacteria develop antimicrobial resistance through various mechanisms. One of the main ones is genetic mutation, which occurs spontaneously in bacterial DNA. Such mutations can give bacteria the ability to survive antibiotics.
- Genetic Mutation: some mutations alter the target of the antibiotic in bacteria, making them insensitive to the drug.
- Genetic Transfer: bacteria can acquire resistant genes from other bacteria through processes such as conjugation.
- Active Efflux: some bacteria develop pumps to expel the antibiotic out of the cells, decreasing its effectiveness.
These processes, combined with the inappropriate use of antibiotics, accelerate the development of antimicrobial resistance.
It is essential to understand these mechanisms in order to develop new treatment and prevention strategies.
Causes of Resistance in the Eyes
Antimicrobial resistance in the specific area of the eyes can be attributed to several factors.
Among the main causes are the overuse of antibiotics and recurrent eye infections, which contribute significantly to aggravating the problem.
Misuse of Antibiotics
The overuse and misuse of antibiotics is one of the main causes of antimicrobial resistance. Often, patients receive antibiotics even when they are not needed at all, such as in the case of viral infections.
In summary:
- Frequent use of antibiotic eye drops to treat minor infections can lead to resistance.
- Prescribing broad-spectrum antibiotics increases the risk of resistance development.
- Self-medication, without consulting a doctor, amplifies the problem.
Indeed, it is essential to educate patients on the correct use of antibiotics and to encourage health professionals to follow appropriate prescribing guidelines.
With regard to the target audience for antibiotics, the WHO has repeatedly stressed the need to reduce the use of broad-spectrum antibiotics (WATCH), which are more likely to induce microbial resistance, in favour of narrow-spectrum antibiotics (ACCESS).
The recommended goal is to bring the use of ACCESS antibiotics in common uncomplicated infections to 70%. Unfortunately, most countries, even within the European Union itself, are far from this goal.
To promote education on the responsible use of antibiotics, the AIFA, the Italian Medicines Agency, has made available the Italian version of the guide prepared by the WHO, the AWARE manualwhich can be downloaded from this link Antibio Manual (Access, Watch, Reserve) - Italian edition of 'The WHO AWare Antibiotic Book'.
Recurrent Eye Infections
Recurrent eye infections may contribute to antimicrobial resistance. Indeed, when eye infections recur frequently, patients often receive repeated antibiotic treatment.
These repeated courses of treatment may have the side effect of selecting resistant bacterial strains, making future infections more difficult to treat.
Causes of recurrent infections include:
- Poor eye hygiene.
- Improper use of contact lenses.
- Work environment or personal habits that increase the risk of infection.
In order to reduce the incidence of these infections, it is essential to promote the knowledge and dissemination of proper hygiene practices and, in parallel, to make people responsible for proper contact lens wear.
Warning Signs Not to Be Ignored
Recognising the symptoms of antimicrobial resistance and obtaining an early diagnosis of infections is crucial to prevent errors in the selection and management of the most correct and effective therapy.
Knowledge of warning signs and advanced diagnostic methods can facilitate early intervention.
It is important to be aware of the signs that might indicate a resistant infection.
Among the most common symptoms are:
- Persistent reddening and swelling of the eyes.
- Unusual, foul-smelling eye secretions.
- Eye pain that does not respond to standard treatments.
If you notice these symptoms, it is essential to consult a doctor 0culist as soon as possible. An accurate diagnosis is essential to determine the appropriate treatment and improve the chances of recovery.
Advanced Diagnostic Methods
Advances in medical technology have led to more precise diagnostic methods to identify resistant eye infections. These tests include:
- Sensitivity testing: They make it possible to identify which antibiotics are effective against a particular bacterial strain.
- PCR (Polymerase Chain Reaction): Used to rapidly identify resistance genes in bacteria.
- Microbial Cultures: They allow specific ocular pathogens to be isolated and identified.
These advanced techniques allow ophthalmologists to customise treatments and reduce inappropriate use of antibiotics. Implementing these methods in daily clinical practice can significantly improve the management of eye infections.
Prevention Strategies
Preventing antimicrobial resistance is essential to protect eye health. Effective prevention strategies include good hygiene practices and the use of alternative medications.
- Hygiene and Eye Care
Maintaining good eye hygiene is essential to prevent infections. Here are some recommended practices:
- Wash hands regularly before touching eyes.
- Replace contact lenses and accessories according to the manufacturer's instructions.
- Avoid sharing cosmetics or eye towels.
Following these simple rules can significantly reduce the risk of eye infections and, consequently, the need for antibiotic treatment.
- Alternative Medicines
Besides traditional antibiotics, there are several alternative therapies that can help fight eye infections:
- Natural substances with antimicrobial properties: such as tea tree oil and aloe vera, known for their antibacterial properties.
- Light-based therapies: Techniques such as photodynamic therapy can be effective against some pathogens.
- Ocular probiotics: Studies have shown that applying probiotics directly to the eyes can help reduce pathological bacterial growth.
Incorporating these methods into eye care can provide additional protection against resistant infections, reducing the need for antibiotics.
Role of Research and Health Policy
Research and health policies play a crucial role in controlling antimicrobial resistance. Developing global initiatives and raising public awareness are essential steps to address this challenge.
- Global Control Initiatives
Numerous international organisations are working to combat antimicrobial resistance through various initiatives:
- WHO (World Health Organisation): promotes the rational use of antibiotics and global surveillance of resistant infections.
- Research programmes: through investment in the development of new antibiotics and alternative treatments.
- International Collaborations: countries around the world are joining forces to tackle the problem globally.
These initiatives are crucial to coordinate an international effort to reduce antimicrobial resistance and improve future public health prospects.
- Promoting Public Awareness
Educating the public about the risks of antimicrobial resistance and preventive practices is essential. Awareness-raising campaigns aim to:
- Inform about the correct use of antibiotics.
- Promoting effective hygiene practices.
- Encourage active participation in the fight against microbial resistance.
Many experts in the field emphasise the importance of a holistic approach, taking into account all aspects of the problem:
"Public awareness is one of the most powerful weapons in the fight against antimicrobial resistance."
Creating greater awareness can positively influence the behaviour of individuals and lead to a more responsible use of antibiotics.
On the topic of anti-microbial resistance see also:
- Antibiotic resistance in ophthalmology: update - Oculista Italiano
- Antibiotic resistance: the emergency of the new millennium - Oculista Italiano
- Pharmacists and antibiotic resistance - Oculista Italiano
- Resistant infections: beware of online shopping - Oculista Italiano
- Antibiotic resistance in eye infections - Oculista Italiano
- Asbell P.A. et al. Antibiotic resistance among ocular pathogens in the United States: five-year results from the Antibiotic Resistance Monitoring in Ocular Microorganisms (ARMOR) Surveillance study. JAMA Ophthalmol.
- ESCRS Guidelines for Prevention and Treatment of Endophthalmitis Following Cataract Surgery: Data, Dilemmas and Conclusions 2013.
- Jack D. Stringham et al. Trends in Fluoroquinolone Nonsusceptibility Among Coagulase-Negative Staphylococcus Isolates Causing Endophthalmitis, 1995-2016. JAMA Ophthalmol. 2017.
- Blanco AR et al. Susceptibility of methicillin-resistant Staphylococci clinical isolates to netilmycin and other antibiotics commonly used in ophthalmic therapy. Curr Eye Res. 2013.
- Papa V et al. Ocular flora and their antibiotic susceptibility in patients having cataract surgery in Italy. J Cataract Refract Surg. 2016.
- Sanfilippo C.M et al. Surveillance of the Activity of Aminoglycosides and Fluoroquinolones Against Ophthalmic Pathogens from Europe in 2010-2011. Current Eye Research 2015.
