Retinitis pigmentosa affects thousands of people worldwide with progressive vision loss that, in many cases, begins in childhood and continues to worsen throughout life. It is a complex, often hereditary disease that can significantly affect independence and quality of life. The greatest challenge for the scientific community remains to find treatments that can not only slow down visual decline, but also protect and preserve healthy retinal cells.
In recent years, however, encouraging new perspectives have emerged. Recent studies are revealing innovative molecules capable of stabilising a key protein involved in retinal degenerative processes. This discovery could pave the way for revolutionary targeted therapies capable of directly intervening in the biological mechanisms that lead to vision loss. For many people suffering from retinitis pigmentosa, these results represent a glimmer of hope for a future in which the progression of the disease can finally be controlled.
Find out how research is transforming the understanding of this disease and what new therapeutic possibilities may soon become a reality.
What is Retinitis Pigmentosa?
Retinitis pigmentosa is a genetic disorder that affects the retina, the membrane that lines the inner postero part of the eyeball and is responsible for converting light into electrical signals that are interpreted by the brain as images. The condition develops when photoreceptors - the specialised cells that enable us to see in the dark (rods) and distinguish colours and details (cones) - begin to degenerate.
This degeneration progresses slowly but continuously, leading to changes in visual perception.
Although there are many forms and causes, early diagnosis allows the evolution of the disease to be monitored and personalised strategies to be adopted to preserve eye function as much as possible.
Symptoms and Disease Progression
The symptoms of retinitis pigmentosa can vary significantly from person to person, depending on the genetic mutation involved and the age of onset. Despite this variability, some signs are common. The first difficulties often involve night vision, which may be followed by problems moving around in dimly lit environments or with strong light contrasts.
Another characteristic symptom is the gradual loss of peripheral vision: the visual field tends to narrow, eventually creating a kind of 'tunnel vision'. This change may go unnoticed in the early stages, but with time it becomes more noticeable and significantly limits the perception of side obstacles.
Many people notice that they stumble more easily or have problems moving in unfamiliar environments.
Progression can be slow, taking years or decades, or advance more rapidly, making each case unique in its course.
In advanced stages, central vision can be impaired, making activities such as reading, driving or recognising faces difficult. Although there is currently no definitive cure, understanding how the disease evolves over time allows targeted measures to be taken to preserve vision for as long as possible, using visual aids, assistive technology and regular check-ups.
Research continues to offer new hope, with gene therapies, innovative molecules and personalised approaches that could radically change the experience of people with retinitis pigmentosa.
Genetic Mutations and Rhodopsin Malformations
The role of genetic mutations in retinitis pigmentosa is central and one of the most studied fields in recent years. Understanding how specific genetic alterations interfere with the functioning of rhodopsin, a key protein in visual processing, is essential for developing more effective therapies.
Pathogenic Related Mutations
The mutations responsible for retinitis pigmentosa are often linked to inherited genetic defects that directly affect the structure and function of rhodopsin. This protein, present in the rods of the retina, is indispensable for the eye to perceive light, especially in low-light conditions.
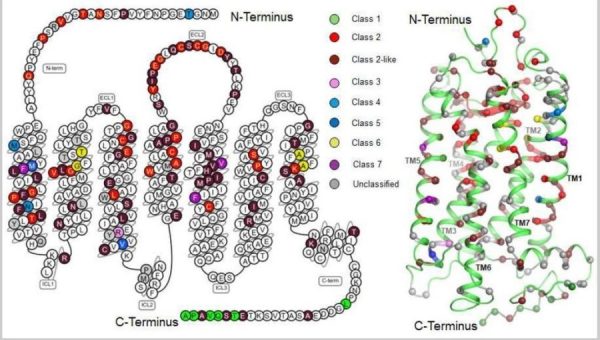
When a mutation alters the structure of rhodopsin, the protein can misfold, become unstable or fail to reach its position correctly in photoreceptor cells. This malfunction triggers a cascade of cellular events that gradually damage the photoreceptors.
Genetic mapping of these mutations has become a fundamental tool as it allows the origin of the defect to be precisely identified, the progression of the disorder to be predicted and, above all, specific therapeutic targets to be identified. Knowing the precise mutation also helps guide patients towards clinical trials and personalised therapies.
Effects of Malformations on Sight
Alterations in rhodopsin have profoundly debilitating effects on vision, as they impair the eye's ability to convert light into nerve impulses. Without a functioning rhodopsin, photoreceptors enter a state of constant stress, lose functionality and, over time, undergo cell death.
This degenerative process results in a progressive loss of vision, which often begins with difficulties in night vision and a narrowing of the visual field. As the rods degenerate, the cones - responsible for seeing colours and details - may also be damaged, leading to an overall deterioration of visual capacity.
Understanding how this degeneration occurs is crucial because it allows researchers to develop interventions aimed at stabilising rhodopsin, protecting photoreceptors and slowing down the progression of the disease.
Current Therapeutic Strategies
The treatment of retinitis pigmentosa is evolving rapidly, thanks to the arrival of advanced genetic technologies and new therapeutic molecules. Both experimental approaches, such as gene therapies, and clinical strategies to help patients better live with the disease are currently being explored.
Emerging Genetic Therapies
Gene therapies represent one of the most promising frontiers in the treatment of retinitis pigmentosa. These interventions aim to directly correct the genetic mutation responsible for rhodopsin dysfunction.
Using viral vectors, the researchers succeeded in introducing a corrected copy of the gene into the retina, with the aim of restoring functional production of the protein. Initial clinical studies have shown encouraging results: improvements in light sensitivity and a stabilisation in photoreceptor degeneration.
Although research is still ongoing and treatments are not available for all variants of the disease, gene therapies open up the possibility of tackling the disease before it arises, offering a potentially life-saving approach for many patients.
Clinical Management Options for Patients
Alongside genetic therapies, there is a wide range of clinical and support options for those living with retinitis pigmentosa.
These approaches include:
- advanced visual aidssuch as filter lenses, digital magnifiers and electronic devices that improve contrast and facilitate mobility;
- psychological supportwhich is essential to cope with the emotional impact of progressive vision loss;
- visual rehabilitation programmeswhich help patients maintain autonomy in daily activities.
A multidisciplinary team - consisting of ophthalmologists, geneticists, vision therapists, psychologists and rehabilitation counsellors - is essential to create a personalised management plan and update the patient on emerging treatment options.
New Research Breakthroughs
 Scientific research is going through a phase of enormous progress, thanks to advanced computational techniques, more accurate animal models and new molecules designed to stabilise rhodopsin. These discoveries are rapidly changing the therapeutic outlook for retinitis pigmentosa.
Scientific research is going through a phase of enormous progress, thanks to advanced computational techniques, more accurate animal models and new molecules designed to stabilise rhodopsin. These discoveries are rapidly changing the therapeutic outlook for retinitis pigmentosa.
Virtual Screening and Corrective Molecules
Virtual screening is one of the most innovative tools used recently. Through advanced algorithms, researchers can simulate thousands of interactions between potential therapeutic molecules and the mutated rhodopsin, identifying the most promising ones in correcting structural defects.
Recent studies have identified two non-retinoid compounds with the ability to cross the blood-retinal barrier and stabilise malformed rhodopsin. These molecules appear to prevent photoreceptor degradation, paving the way for new pharmacological treatments applicable to different clinical forms of rhodopsin-related retinitis pigmentosa.
Impact of New Discoveries on Animal Models
Animal models continue to be an invaluable resource for testing the efficacy of new therapies. In mice genetically predisposed to developing retinal lesions in response to bright light, corrective molecules have been shown to protect the retina and prolong photoreceptor survival.
These results not only confirm the therapeutic potential of the new molecules, but also highlight the possibility of applying these approaches on a larger scale. If the data are successfully replicated in humans, we could see a radical change in treatment strategies for retinitis pigmentosa.
Importance of Genetic Diagnosis
Genetic diagnosis is a cornerstone in the management of retinitis pigmentosa. Identifying the mutation responsible makes it possible to
- define the prognosis more precisely,
- choose targeted therapeutic strategies,
- participate in specific clinical trials,
- access to genetic counselling programmes for family members.
Early diagnosis, especially in individuals with a family history of the disease, can significantly improve both clinical management and treatment opportunities.
Treatment Perspectives for Patients
Treatment prospects for retinitis pigmentosa are changing faster than ever before. Thanks to the advancement of gene therapies, the discovery of corrective molecules and the development of increasingly sophisticated assistive technologies, patients can expect increasingly effective options.
The objective, in the coming years, is twofold:
- preserve sight for as long as possible,
- significantly improve quality of life.
Staying informed about scientific advances and maintaining a continuous dialogue with specialised centres is essential to make the most of new developments.
- Ortega JT, Gallagher JM, McKee AG, et al. Discovery of non-retinoid compounds that suppress the pathogenic effects of misfolded rhodopsin in a mouse model of retinitis pigmentosa. PLoS Biol. 2025 Jan 14;23(1):e3002932. doi: 10.1371/journal.pbio.3002932.
- Pashandi Z, Jastrzebska B. Small-Molecule Ligands of Rhodopsin and Their Therapeutic Potential in Retina Degeneration. Int J Mol Sci. 2025 Sep 15;26(18):8964. doi: 10.3390/ijms26188964.
