Diabetes mellitus is now a global emergency and the eye is one of the organs that can be most severely affected by its complications. Prevention, early diagnosis and appropriate treatment are our most important resources for combating it.
Diabetes mellitus
 diabetes mellitus comprises a group of common metabolic disorders resulting from a decrease in insulin activity, secondary to reduced availability of this hormone, an impediment to its normal action or a combination of the two1.
diabetes mellitus comprises a group of common metabolic disorders resulting from a decrease in insulin activity, secondary to reduced availability of this hormone, an impediment to its normal action or a combination of the two1.
A distinctive feature of diabetes mellitus is thehyperglycaemiawith which, with the passage of time, certain complications are associated: macrovascular alterations, which consist of the development of particularly severe and early atherosclerosis, and microvascular alterations, i.e. alterations in the microcirculation specific to diabetic disease, which become particularly manifest in the retina, kidney and nervous system.
Epidemiological data predict a dramatic increase in the prevalence of diabetes in Europe, from 55 million in 2010 to over 66 million in 2030.
WHO forecasts on the future prevalence of diabetes mellitus in the various regions of the world predict substantial increases in industrialised countries, but especially in developing countries, where easier access to food sources and the simultaneous reduction in energy expenditure will favour the increase in the disease.
Classification
The two most important categories of DM include type 1 and type 2 diabetes.
Type 1 diabetes

It is the consequence of total or near-total insulin deficiency. In the majority of cases, type 1 diabetes is the immune-mediated form. In approximately 90% of type 1 diabetics, at the onset of the disease, the presence in the plasma of autoantibodies directed against the pancreatic β-cells that produce insulin can be shown to be the cause of their destruction. In this form of diabetes, in which there is an almost absolute deficiency of insulin, this hormone must be administered as replacement therapy. This is why type 1 diabetes was formerly referred to as insulin-dependent diabetes or childhood diabetes, given its onset generally before the age of 30.
Type 2 diabetes
It is a heterogeneous group of alterations characterised by varying degrees of insulin resistance, impaired insulin secretion and increased glucose production. It represents the most common form of diabetes (approximately 90% of the total diabetic population), and is preceded by an early phase of altered glucose homeostasis, defined as glucose intolerance. At this stage, hyperglycaemia can be controlled by a combination of behavioural measures, such as diet and exercise, and medical treatment, with drugs that increase peripheral insulin sensitivity or reduce hepatic glucose production. In the past, this form of diabetes was called non-insulin-dependent or adult-onset or maturity diabetes; this term has now become obsolete as many individuals with type 2 diabetes eventually require insulin treatment to control blood glucose. Furthermore, although it more typically develops with advancing years, it is now more frequently diagnosed in children and young adults, particularly obese adolescents with a sedentary lifestyle.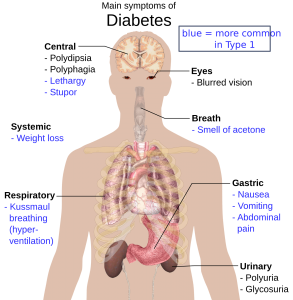
The increasing prevalence of obesity is a critical factor associated with the growing number of people with diabetes; in particular, the prevalence of type 2 diabetes appears to be growing in parallel with the increase in the world obesity rate.
Ocular complications of diabetes mellitus
Some of the most serious eye diseases that can affect diabetic patients are: diabetic retinopathy, diabetic macular oedema, which sometimes occurs precisely as a complication of diabetic retinopathy, glaucoma and cataracts.
Diabetic retinopathy
Diabetic retinopathy is one of the leading causes of blindness in the world and its prevalence is expected to double in the next decade. The onset of this disease in diabetic patients is linked to high blood glucose levels, which induces damage to the retinal microcirculation.
A correct classification of diabetic retinopathy is essential in order to direct the choice of the most appropriate therapy and determine the prognosis of the disease.
In a study of patients with type 2 diabetes, it was found that there are three phenotypes by which to classify different types of retinopathy: A, B and C. Type C has the highest risk of worsening, as well as a greater likelihood of developing complications that can severely impair vision. Phenotype A, on the other hand, presents the lowest risk of worsening and development of complications.
This is why correct diagnosis and classification of this pathology are so important. Today, it is possible to use tests that are quite simple to perform, such as colour photography of the fundus and optical coherence tomography, which can be repeated without great inconvenience for the patient or difficulty for the clinical staff. In fact, one must bear in mind that any person with type 1 or type 2 diabetes or gestational diabetes (the form of diabetes that can occur during pregnancy) can develop a form of diabetic retinopathy.
Glaucoma
Glaucoma is a chronic, progressive eye disease that results in irreversible damage to the optic nerve, the main cause of which is identified as elevated intraocular pressure (IOP).
Glaucoma is characterised by the gradual and progressive death of retinal ganglion cells and is one of the leading causes of irreversible vision loss worldwide.
An association between diabetes and glaucoma has been demonstrated, particularly with primary open-angle glaucoma (POAG), which is in fact the most frequent form of glaucoma diagnosed in individuals with diabetes and, in general, the most common type in the population.
Risk factors
The main risk factors for primary open-angle glaucoma include:
- Advanced age
- Positive family history for the disease
- African ethnicity
- Thinning of the central corneal thickness
- Systemic arterial hypertension
- Diabetes
- Myopia
Cataracts
Diabetes affects all ocular structures, but the crystalline lens and retina are undoubtedly among the ocular districts that can be most significantly affected.
Osmotic, refractive and accommodative alterations of the crystalline lens have been demonstrated in diabetic patients, as well as an increased risk of cataracts, since cataracts arise precisely as a result of opacification of this ocular structure.
Cataracts, along with diabetic retinopathy and glaucoma, are also a major cause of blindness worldwide.
Prevention through close monitoring of haematological parameters, early diagnosis and timely treatment can be decisive in preserving visual function in people with diabetes.
For this reason, all diabetic patients, but especially the elderly, should visit an ophthalmologist regularly to diagnose and treat any ocular complications related to this serious systemic disease in a timely manner.
World Health Organisation (2022, September 16th) https://www.who.int/news-room/fact-sheets/detail/diabetes
Diabetes and Vision Loss (2022, December 19th). Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/managing/diabetes-vision-loss.html
Diabetic Eye Disease (2023, February 10th). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/diabetic-eye-disease
Diabetic Retinopathy: Causes, Symptoms, Treatment (2022, September 9th). American Academy of Ophthalmology. https://www.aao.org/eye-health/diseases/what-is-diabetic-retinopathy
Marqués, I. P., Madeira, M. H., Messias, A. L., Martinho, A. C. V., Santos, T., Sousa, D. C., Figueira, J., & Cunha-Vaz, J. (2020). Different retinopathy phenotypes in type 2 diabetes predict retinopathy progression. Acta Diabetologica, 58(2), 197-205. DOI: 10.1007/s00592-020-01602-9
Diabetes and risk of glaucoma: systematic review and a Meta-analysis of prospective cohort studies. (2017, 18 Septiembre). International Journal of Ophthalmology. https://doi.org/10.18240/ijo.2017.09.16
Rhee, D. J. (2023, 6 febrero). Primary-open-angle . Manual MSD versión para profesionales. https://www.msdmanuals.com/professional/eye-disorders/glaucoma/primary-open-angle-glaucoma
Silva Pacheco, M., & Chacón Chavez, K. (2020). Diabetes mellitus type 2: Cambios densitométricos del cristalino. Rev DigitPostgrade. 9(1): e187. DOI: 10.37910/RDP.2020.9.1.e187
