The amniotic membrane: a valuable resource
 The amniotic membrane is a valuable resource for reconstructive surgery of the ocular surface, which is increasingly being used in serious diseases of the cornea, limbus and conjunctiva when they do not respond to traditional local therapies.
The amniotic membrane is a valuable resource for reconstructive surgery of the ocular surface, which is increasingly being used in serious diseases of the cornea, limbus and conjunctiva when they do not respond to traditional local therapies.
Limits of use
One of the most important limitations to the therapeutic use of cells and tissues in the ophthalmic field has always been the limited availability of surgical rooms in which to carry out therapies in sterility and safety. In order to alleviate the onerous logistical tasks involved in preparing, storing and reactivating amniotic tissue, Andrew Hopkinson of the University of Nottingham (UK) has developed an innovative technique to process and store amniotic tissue.
The Hopkinson technique
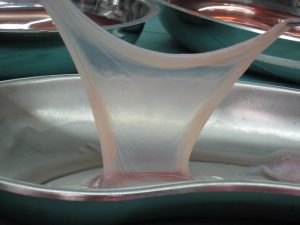
This technique, which has also been patented, involves a vacuum drying process to produce a dry matrix, derived from human amniotic membrane, to be used in the eye as a bandage, graft or as part of a contact lens bandage, which serves to keep the amniotic tissue in situ.
Areas of use
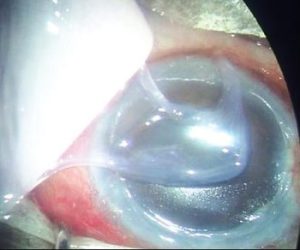 In the surgical field, this amniotic membrane derivative proved invaluable in the case of patients who had to undergo epithelial redirection to treat a limbus stem cell deficiency (LSCD) resulting from stem cell transplantation.
In the surgical field, this amniotic membrane derivative proved invaluable in the case of patients who had to undergo epithelial redirection to treat a limbus stem cell deficiency (LSCD) resulting from stem cell transplantation.
Harminder S. Dua and his team of researchers treated patients with LSCD resulting from ocular chemical burn, keratopathy related to congenital aniridia and other ocular surface lesions. Vacuum-dried amnion and fibrin glue were used as part of a conjunctivo-epithelial redirection technique. Amniotic membrane was used instead of autotransplantation of conjunctival tissue in the surgical treatment of pterygium, with a sutureless procedure requiring a shorter operating time.
Tolerance and safety of the amniotic membrane
Contact lens-mounted amniotic membrane was found to be well-tolerated by patients with acute chemical burns to the eyes, and Lotfy NM et al reported data from 21 patients (23 eyes) with acute chemical burns to the eyes, who were treated urgently and, within two days, had amniotic tissue applied.
Five of the treated eyes underwent repeated lens fitting and the extent of epithelial injury was reduced after the second fitting.
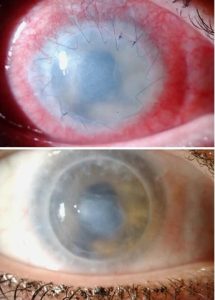 Complete healing of the epithelium was achieved in all eyes within 1 month.
Complete healing of the epithelium was achieved in all eyes within 1 month.
Properties of the amniotic membrane
Amniotic membrane is a tissue with unique properties and can be exploited for numerous ocular applications, with the advantage that it can be applied without sutures. It is stable at room temperature and can be stored at temperatures between 2° C and 25° C.
Furthermore, with regard to vacuum-dried tissue, the rehydration of the dried membrane is almost instantaneous, a quality that makes it usable with a rather short preparation time.
An Italian study, 'Human amniotic membrane plug to promote failed macular hole closure'It also tested its use for plugging recurrent macular holes, i.e. its use in restorative retinal surgery.
See also
- Dua HS, Ting DSJ, AlSaadi A, Said DG. Management of limbal stem cell deficiency by amnion-assisted conjunctival epithelial redirection using vacuum-dried amniotic membrane and fibrin glue. Br J Ophthalmol. 2023;107(3):342-348. doi:10.1136/bjophthalmol-2020-318496
- Xanthopoulou PT, Elanwar M, Alzyadi M, Lavaris A, Kopsachilis N. Α novel sutureless pterygium excision surgery using human-derived dehydrated amniotic membrane. Cureus. 2022;14(4):e23839. Published 2022 Apr 5. doi:10.7759/cureus.23839.
- Lotfy NM, Al Rashidi S, Hagras SM. Clinical outcomes of vacuum-dehydrated amniotic membrane (Omnigen) mounted on contact lens (Omnilenz) in eyes with acute chemical eye injuries. Graefes Arch Clin Exp Ophthalmol. 2023;261(12):3541-3547. doi:10.1007/s00417-023-06151-9
- Caporossi T, Pacini B, Bacherini D, Barca F, Faraldi F, Rizzo S. Human amniotic membrane plug to promote failed macular hole closure. Sci Rep. 2020;10(1):18264. Published 2020 Oct 26. doi:10.1038/s41598-020-75292-2
