Fluocinolone acetonide has now become an authorised therapeutic option for the treatment of non-infectious uveitis.
Uveitis is an inflammation of the uvea, the intermediate tunic of the eyeball, interposed between the sclera and the retina.
This disease can be classified according to its course, acute or chronic, or according to its cause, which can be infectious or non-infectious.
If the cause is infectious, uveitis will be due to the presence of viruses or bacteria; if the cause is non-infectious, on the other hand, uveitis is often associated with autoimmune disorders.
Classification
Depending on the area affected, a distinction can be made:
- anterior uveitis;
- intermediate uveitis;
- posterior uveitis;
- panuveiti.
Symptoms
 The main symptoms include loss of visual acuity e increased retinal thickness.
The main symptoms include loss of visual acuity e increased retinal thickness.
The lack of adequate and timely treatment can also lead to serious complications.
In particular, uveitis affecting the posterior segment may lead to macular oedema, irreversible reduction of visual capacity and blindness.
Non-infectious uveitis
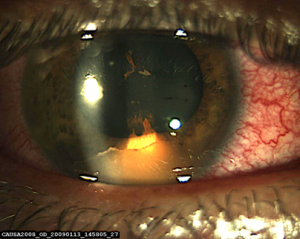 Although an uncommon group of diseases, uveitis causes 5-20% of legal blindness in the United States and Europe. In non-infectious forms of uveitis, the decline in visual acuity is often linked to the presence of macular oedema, vitritis or inflammation of the optic nerve.
Although an uncommon group of diseases, uveitis causes 5-20% of legal blindness in the United States and Europe. In non-infectious forms of uveitis, the decline in visual acuity is often linked to the presence of macular oedema, vitritis or inflammation of the optic nerve.
Choice of treatment
The choice of the most appropriate treatment is based on the clinical features of uveitis in each patient, associated with the degree of inflammation, extent of visual impairment, and available scientific evidence.
The aim is to choose the best possible treatment to achieve maximum therapeutic effect with minimum risk of complications and side effects. Using these principles of therapy, it is possible to choose single or combined treatments, different doses and different routes of administration.
The patient's age, co-morbidities and the location of the uveitis (local or systemic, mono- or bilateral, anterior, intermediate or posterior) also play a role in the choice of therapy.
Eye structure and therapy
The ocular structure is an important factor limiting the diffusion of drugs into the different ocular segments. The aim is to achieve and maintain therapeutic drug concentrations at the level of the ocular segment most affected by inflammation.
The blood-retinal barrier
The retina and vitreous are, in fact, separated from the blood circulation by the blood-retinal barrier which limits the diffusion of systemically administered drugs into these districts. The outer part of the blood-retinal barrier is formed by the occluding junctions of the retinal pigment epithelium, and the inner part by the occluding junctions of the endothelium of the retinal capillaries. These barriers, which limit the diffusion of drugs, have led to the search for different therapeutic approaches to drug delivery for retinal and vitreous diseases.
Several strategies have been adopted to achieve adequate therapeutic concentrations at the level of the posterior segment, and the intravitreal route of administration, which allows several substances to be injected into the vitreous chamber, has proven to be among the most effective.
Relapse prevention
For the prevention of recurrence of recurrent non-infectious uveitis affecting the posterior segment of the eye, a drug based on the active ingredient Fluocinolone Acetonide (FAc), belonging to the corticosteroid category, already authorised for the treatment of diabetic macular oedema (EMD).
Fluocinolone acetonide and extended-release implant
 Fluocinolone acetonide is a corticosteroid characterised by low water solubility and high fat solubility, also having the same anti-inflammatory activity as dexamethasone.
Fluocinolone acetonide is a corticosteroid characterised by low water solubility and high fat solubility, also having the same anti-inflammatory activity as dexamethasone.
The slow-release, long-lasting, non-biodegradable insert, containing fluocinolone acetonide 190 μg, was approved in Italy for the treatment of chronic diabetic macular oedema that does not sufficiently respond to other available therapies, and the indications were subsequently extended to non-infectious uveitis.
Three-year coverage
The drug is administered via the slow-release intravitreal route. The implant allows a low, but continuous dose of steroid to be administered with a drug coverage for up to 3 years.
This results in a reduction in the number of intravitreal injections to which the subject should be subjected in the case of drugs with a shorter duration of efficacy of the insert.
Fluocinolone acetonide: efficacy and safety
According to a clinical study on the efficacy and safety of this drug, in the first 3 months after implantation it was determined that an improvement in visual acuity and a decrease in retinal thickness in 82% and 100% of the treated eyes, respectivelyduring the first three months of follow-up.
In the following months of follow-up, a significant improvement in inflammation was observed in 82% of the treated eyes, and only 36% presented a recurrence.
Fluocinolone acetonide: Side effects
The most common side effects encountered were increased intraocular pressure and cataract formation, however with a manageable safety profile and a risk/benefit ratio in favour of the latter.
Conclusions
The undisputed advantages of this device are, therefore, the long-term release of the drug and the fact that it can be injected into the vitreous with a minor surgical procedure, as opposed to other treatment options.
On the subject of non-infectious uveitis and macular oedema see also:
- Non-infectious uveitis: classification and treatment - Oculista Italiano
- Diabetic macular oedema: safety and availability of steroid drugs - Oculista Italiano
- Weber L.F. et al. Injectable 0.19-mg fluocinolone acetonide intravitreal implant for the treatment of non-infectious uveitic macular oedema. J Ophthalmol Inflamm Infect 2019; 9:3. https://doi.org/10.1186/s12348-019-0168-9
- Chen S.C., Sheu S.J. Recent advances in managing and understanding uveitis. F1000Res. 2017; 6:280.
